The need for rapid point-of-care Peripheral Arterial Disease (PAD) screening tools in healthcare facilities
What is PAD?
Peripheral arterial disease (PAD) affects more than 200 million adults worldwide and is the manifestation of atherosclerosis in the lower limbs that can impair mobility. It’s a narrowing of the peripheral arteries that carry blood away from the heart to other parts of the body. The most common type is lower-extremity PAD where blood flow is reduced to the legs and feet. It’s a condition difficult to diagnose and detect by healthcare professionals as PAD symptoms are often mistaken for other things.
Early detection and intervention is key because PAD is a risk factor for coronary artery disease (CAD) and cerebrovascular disease (CVD). Left untreated, can lead to gangrene, leg or foot amputation, even heart attacks and stroke.
Using NIRS to See Underlying Vascular Disease
PAD can be diagnosed noninvasively with a segmental blood pressure measurement and calculating an ankle-brachial index (ABI) or toe-brachial index (TBI). ABI is the systolic blood pressure obtained at the ankle divided by the systolic blood pressure obtained at the brachial artery while the patient is lying down. A ratio of less than 1 (typically defined as ≤ 0.9) is considered abnormal and used to define PAD. In clinical settings, resting ABI is the most commonly used measurement to detect PAD but variation in measurement protocols can lead to differences in ABI values obtained.
With near-infrared spectroscopy (NIRS), healthcare providers can assess patients’ microvascular status and get accurate measurements on recovery time, deoxygenation, oxygen consumption, tissue oxygen saturation, and total hemoglobin. Because microvasculature is not visible to the eye, utilizing rapid point-of-care diagnostic tools in healthcare facilities is valuable in screening for PAD. They can also be useful with assessing how effective a certain treatment is helping with preventing deteriorating patients with PAD.
Using near-infrared light (600nm-1000nm), SnapshotNIR can detect tissue oxygenation saturation which is one of the key indicators of tissue health. Physicians can use diagnostic tools like the SnapshotNIR to see below the surface at the microvasculature network and perfusion characteristics in tissue.
“I found this to be a very useful tool in my experience. It’s very easy to use,” says Dr. Craig Walker, interventional cardiologist and founder of the Cardiovascular Institute of South Houma. “In the past, that was hard to get: easy-to-use devices that give us easily reproducible information. This device has become my go-to evaluation tool prior to and following a critical limb ischemia intervention. I found the device to be a vital tool in longitudinal follow-up of patients with critical peripheral arterial disease.”
Case Study
A recent case study from Erin Buchness presents a patient while at Mercy Hospital who sustained a fall with bilateral open reduction fixations of her right and left malleolar fractures completed. The patient’s bilateral incisions dehisced prompting multiple rounds of oral and intravenous antibiotics and surgical incision and drainage of her incision sites. She had comorbidities of Type 2 diabetes, coronary artery disease, peripheral arterial disease, peripheral vascular disease, and smoking history. Interventions included a bilateral arterial duplex, a left leg balloon angioplasty of the entire superficial femoral artery and proximal popliteal artery, an angioplasty of left tibioperoneal trunk and right common iliac artery, and a bilateral lower extremity angiogram. Post-interventions, the patient was reimaged with SnapsnotNIR at the foot and ankle sites and images showed a greater than 15 percent increase in tissue oxygenation compared to prevascular intervention procedures.
Using Snapshot, this patient’s bilateral feet, and possibly her legs, were preserved and the team diagnosed her severe peripheral arterial disease and set up a care plan involving cardiovascular interventions, hyperbaric oxygenation therapy (HBOT), and advanced wound care.
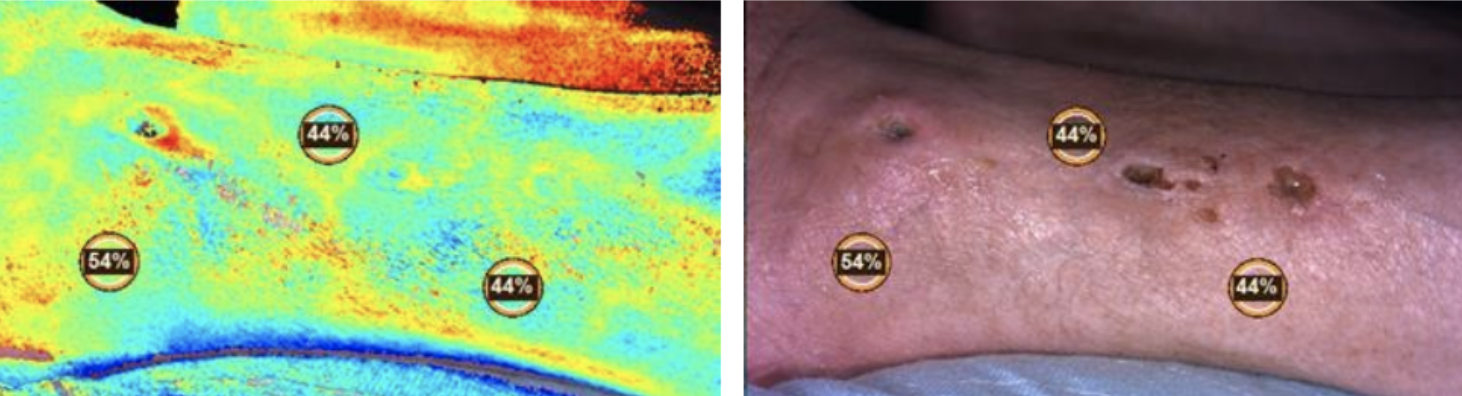
Buchness Case study: Baseline image pre-vascular surgery and arterial doppler showing peripheral arterial ulcer.
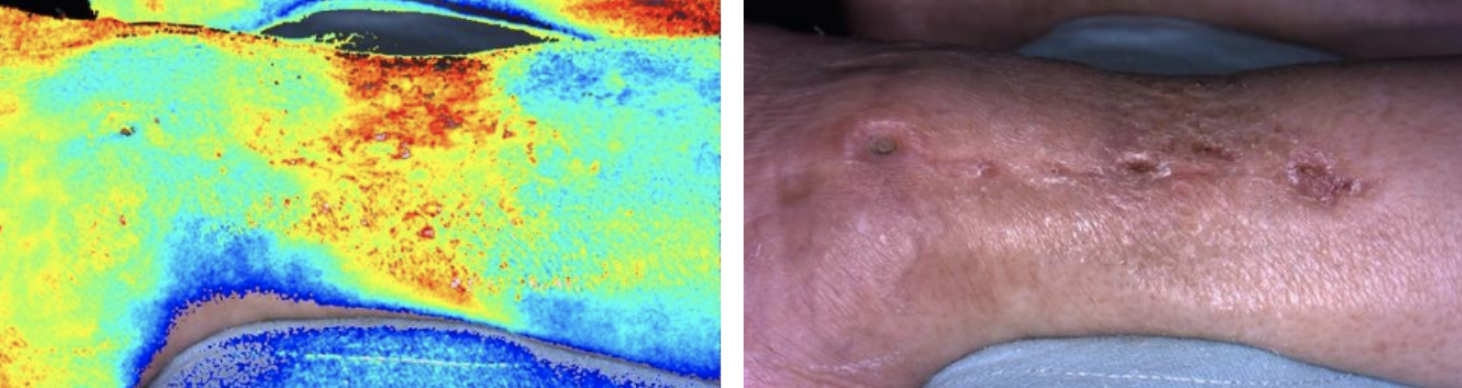
Buchness Case study: Thirteen (13) days following vascular surgery and arterial doppler.
NIRS is a safe, non-invasive technology that generates timely accurate data very quickly and images that can be easily integrated into a patient’s electronic medical record. SnapshotNIR is a cost-effective screening and diagnosis tool that can help physicians make faster and effective decisions so that patient outcomes are improved.
https://www.heart.org/en/health-topics/peripheral-artery-disease/pad-toolkit
https://www.aafp.org/pubs/afp/issues/2018/1215/od1.html