Detecting Danger: The Role of Patient Awareness and Physician Screening for Peripheral Arterial Disease
For how prevalent peripheral arterial disease (PAD) is, few clinics and even fewer patients are on the lookout for the signs and symptoms of this slow burning disease.
Doctors’ practices and days are filled with differential diagnoses, referrals, and documentation. Being able to speak about certain signs and symptoms can help the process of assessment and diagnosis for diseases like PAD. As a patient, knowing the right symptoms to be aware of and having that information to bring to doctors appointments can make all the difference when determining next steps of care.
What is PAD?
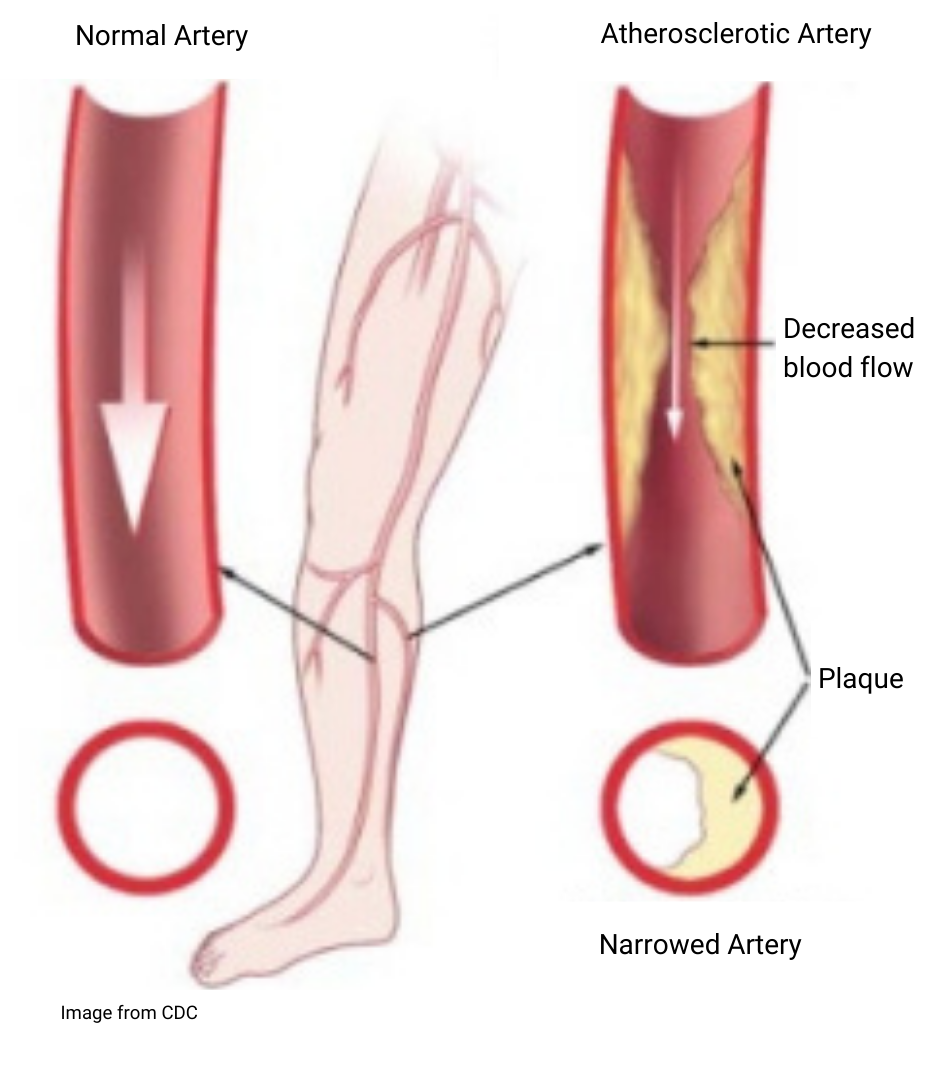
Peripheral arterial disease is a condition that impacts the arteries - blood vessels that travel away from the heart - that carry oxygen-rich blood to our limbs and everywhere in between (1). When these blood vessels become narrowed, stiff, clogged, or blocked, it can cause critical issues (1).
How likely is it to develop PAD?
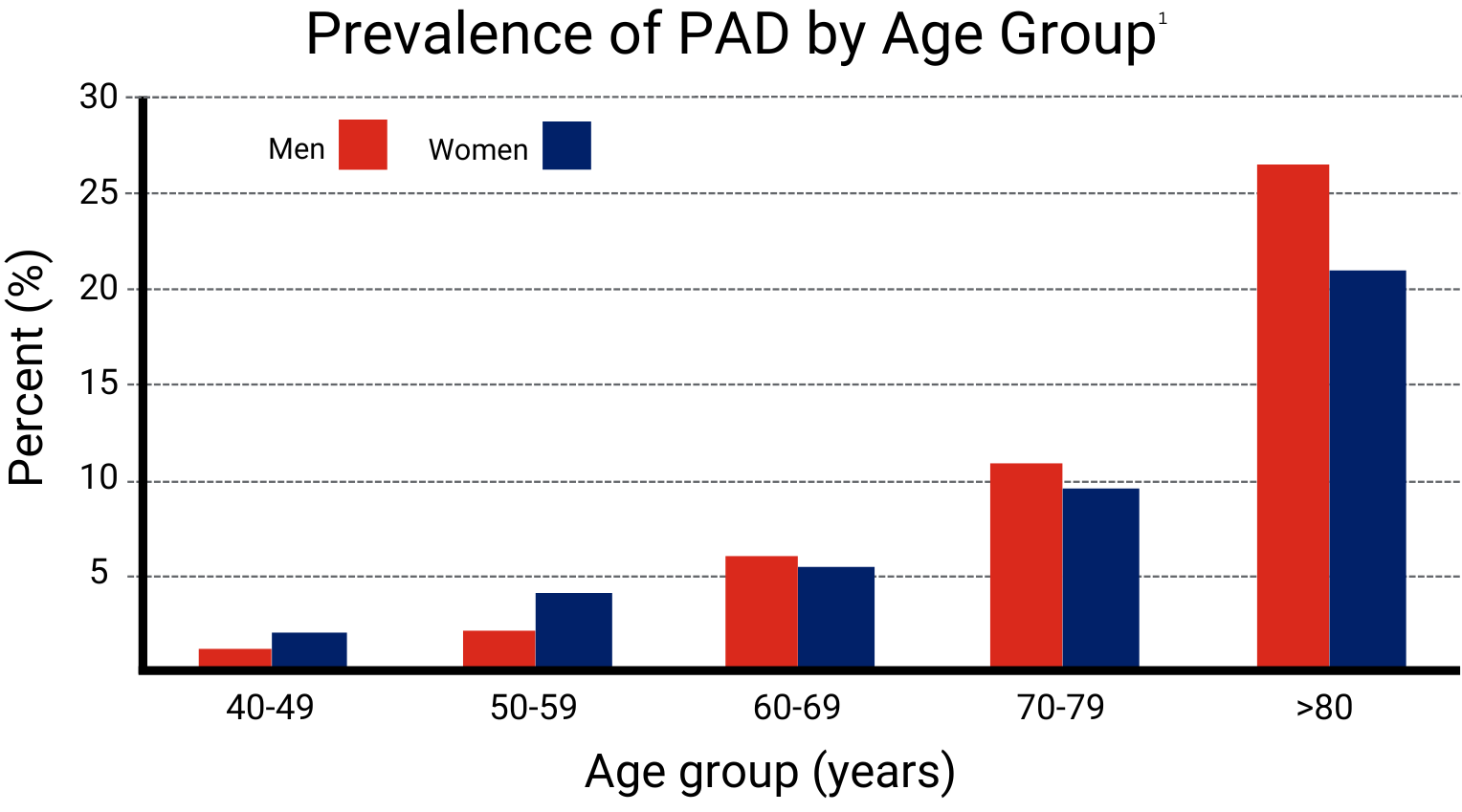
The disease becomes increasingly prevalent as we age, almost doubling per decade after 40 years of age (2). The condition is more common in males than females, and more common in African Americans than Caucasians (2).
What should you look out for?
Monitoring health parameters such as cardiovascular disease risk, smoking, stroke risk, high blood pressure and diabetes are important as these conditions all relate to having a higher risk of developing PAD (1).
Certain symptoms are also worth monitoring and discussing with a doctor. These symptoms include (1):
Intermittent claudication of the legs – pain or numbness
Leg and muscle weakness
Tingling or numbness sensations in the legs
Weak pulses in the legs
Cold extremities
Non-healing wounds
Why does PAD matter?
Things have the potential to go wrong when not diagnosed or identified correctly. PAD can (3):
Impact healing in chronic wounds
Manifest in multiple blood vessels within the legs from the major source arteries in the upper leg, down to the branches that would usually nourish the feet
Progress to what is called critical limb-threatening ischemia (CLTI), a condition that can often result in amputation
Kent Imaging have been assisting physicians in screening patients with a near-infrared imaging spectroscopy (NIRS) device, SnapshotNIR, which measures tissue oxygenation.
Kent works closely with clinics across the US, and in one case, a new patient arrived at a clinic with a slow-to-heal diabetic ulcer that didn’t cause a great deal of concern upon visual inspection. Assessing the blood flow in the leg arteries, it was quickly revealed that, while the patient didn’t have CLTI, they did have significantly lower blood flow than it would appear just by looking at the wound site or feeling for a pulse. This prompted the care team into action for a revascularization procedure that likely saved the patient from needing a foot amputation (†).
What can be done?
Patients can arm themselves with knowledge about the condition and be aware of the risk factors and symptoms that might appear with the disease. Physicians can screen those who are at risk and have action-plans in place for those who are diagnosed with the condition. Technology advances are helping physicians do just that, SnapshotNIR can be used during bedside assessments to help educate patients and streamline referrals.
“The emergence of this piece of technology, where my team can basically take a digital photo and assess circulation, really streamlines our practice and makes it so much easier for us to screen patients.”
Seeing is believing.
NIRS imaging, that uses near-infrared light wavelengths, can look at the small vessels about 2-3mm under the skin, where blood and oxygen are delivered to muscles and tissues. When a patient has PAD, they may have poor blood flow, leading to poor oxygen delivery to the feet. This can be seen in the oxygen saturation image, where the patient’s foot is less red. Red indicates a higher amount of oxygen delivery which is a positive sign, and less red means there is likely not enough oxygen, raising suspicions of conditions like PAD.
“Right at point of care, we can take a picture, and then we can show the patient exactly where any deficits are,” says Dr. Jason Forbes. “So, instead of just giving patients what might be a loose concept of what’s wrong, we can show them, within seconds, where their problem is, where we need to focus to achieve our healing goals, and why we’re asking them to do what we need to do.”
If PAD is caught in time, then surgical planning can be expedited. Surgeons can do procedures to open small or big vessels to reestablish that blood flow, likely leading to a better healing outcome for chronic wounds and reduce the chance of a future amputation, leading to much higher quality of life for the patient.
(†) Read more about how Kent Imaging’s SnapshotNIR is making a difference in patients lives by reading the customer story available here.
References:
(1) Centers for Disease Control and Prevention. “Peripheral Arterial Disease (PAD).” Heart Disease, December 19, 2022. Accessed on March 11, 2024. Available at https://www.cdc.gov/heart-disease/about/peripheral-arterial-disease.html?CDC_AAref_Val=https://www.cdc.gov/heartdisease/PAD.htm
(2) Virani, S.S., Alonso, A., Aparicio, H.J, et al. Heart Disease and Stroke Statistics-2021 Update. A Report from the American Heart Association. Circulation 2021;143(8):e254-743, Chapter 24. https://www.ahajournals.org/doi/epub/10.1161/CIR.0000000000000950
(3) Tran B. Assessment and management of peripheral arterial disease: what every cardiologist should know. Heart 2021;107:1835-1843.