STREAMLINING SUCCESS
With SnapshotNIR, Dr. Jason Forbes and his team are able to deliver higher quality, more efficient care to each and every one of their patients.
Years ago, when Dr. Jason Forbes first began his residency program in Oklahoma, he chose to focus on family medicine because he wanted to pursue a discipline that would allow him to cultivate meaningful and rewarding relationships with his patients.
Then something happened. In his second year of residency, he opted to take an elective in wound care. And in no time, he was hooked.
“I knew, from that very first day, that wound care was what I wanted to do for the rest of my life,” he says. “It had everything I was looking for. You get relationships with patients, and you get to see them regularly, often more regularly than their primary care doctor does. But there’s also a goal, an end point, and it’s very rewarding to work with a patient and have them heal.”
Today, Dr. Forbes is the medical director of the Mercy Wound Care Clinic and Hyperbaric Centre in Springfield, Missouri. There, he leads a small but mighty team of nurses and nurse practitioners who work together to put each of their patients — many of whom are dealing with painful, chronic wounds — on a clear path to healing.
“To work efficiently as a team is our ultimate goal at Mercy Wound Care,” says clinical nurse manager Erin Buchness. “We’ve always stressed an environment of teamwork and no drama in order to maintain an effective patient care model.”
Of course, maintaining such a model also requires buy-in and collaboration from the greater medical community, which Dr. Forbes and his team have in spades.
“We’re part of a program here that has a very supportive and progressive hospital system,” says Dr. Forbes. “In fact, it was one of the vascular surgeons at Mercy Hospital who introduced us to the SnapshotNIR device because he wanted it to be part of our limb preservation protocol.”
Embracing Technology
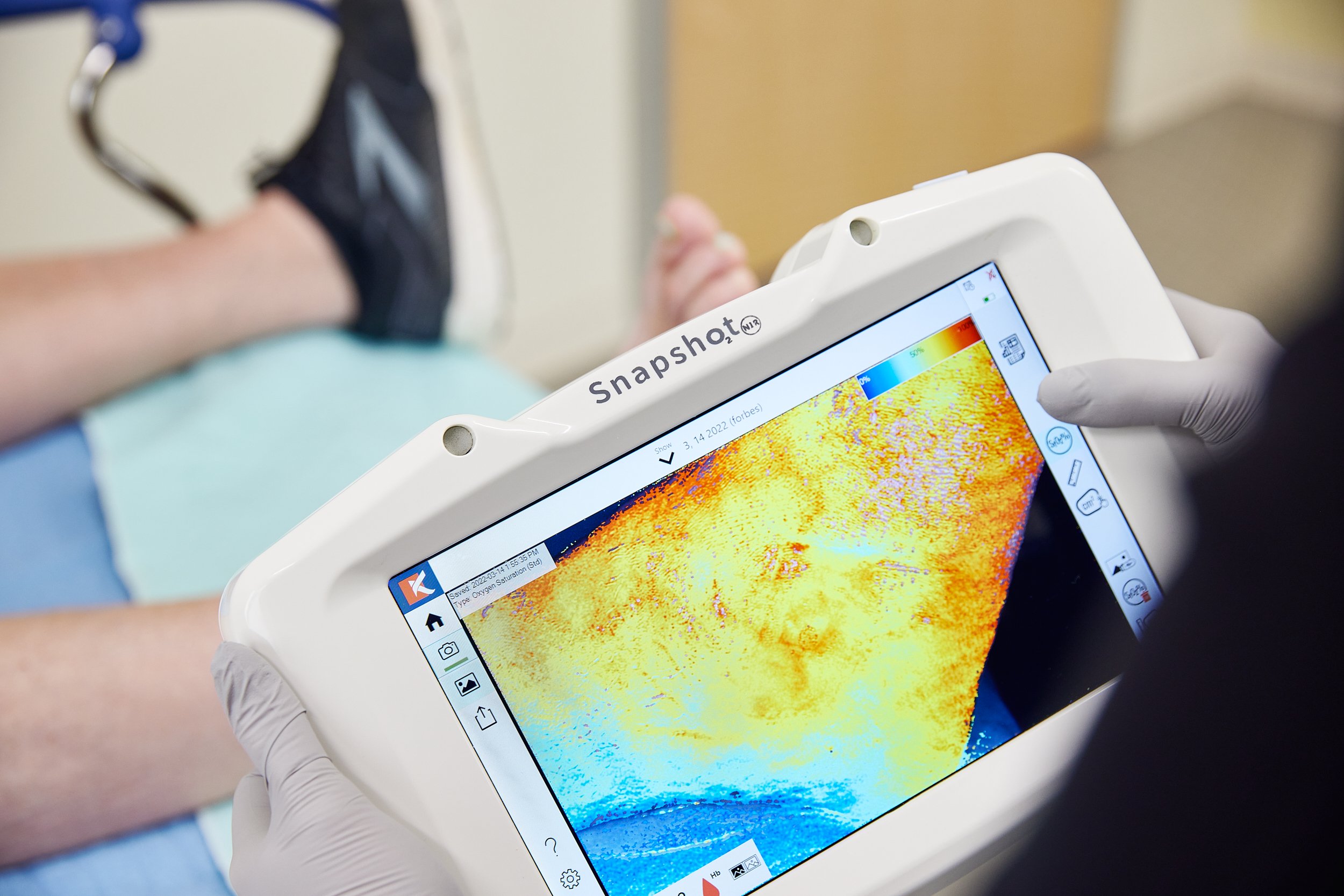
The latest in non-invasive imaging technology, SnapshotNIR is a portable, vascular assessment tool that uses near-infrared (NIR) light to identify the ratio of oxygenated to deoxygenated hemoglobin. As easy to use as a digital camera, SnapshotNIR captures near-instantaneous images that show practitioners the measure of soft tissue oxygenation at a wound site, helping them to determine an appropriate treatment path.
Prior to learning about the device, Dr. Forbes and his team had been relying primarily on older, more time-consuming Doppler assessments and ankle-brachial index testing to determine a patient’s blood flow. SnapshotNIR has been a game-changer.
“One of the things I love about wound care is that there are lots of emerging technologies that can help, and every couple of years there’s something new to get excited about,” says Dr. Forbes. “But for the longest time, there weren’t many breakthroughs in vascular testing — until the Snapshot device. The emergence of this piece of technology, where my team can basically take a digital photo and assess circulation at a wound site, really streamlines our practice and makes it so much easier for us to screen patients.”
Applying Early Intervention
Indeed, it’s now part of their limb preservation protocol that each new patient who comes into Mercy Wound Care with a lower extremity ulcer undergoes SnapshotNIR screening.
“We screen everyone because, while it’s usually obvious if a patient has really bad vascular disease, there have been a handful of patients who I wouldn’t have thought needed vascular intervention until looking at the Snapshot images,” says Dr. Forbes.
In one case, a new patient arrived at the clinic with a slow-to-heal diabetic ulcer that didn’t cause a great deal of concern upon visual inspection. But the intake SnapshotNIR images quickly revealed that, while the patient didn’t have limb-threatening ischemia, he did have significantly lower blood flow than it would appear just by looking at the wound site or feeling for a pulse.
“So, with that Snapshot evidence, we were able to send the patient on to do further vascular testing, and the vascular surgeon was able to revascularize because there wasn’t yet a complete blockage,” says Dr. Forbes. “The patient went on to heal in about eight weeks, as opposed to in the past, when something like that would probably take at least three months because I would treat him, and we would check for infection and do pressure reduction and advanced dressings before looking at the more vascular side of things.’”
In another notable case, the clinic team took in a new patient who had already been revascularized but was still dealing with a chronic ulcer four months after that procedure. Upon studying the SnapshotNIR images of the wound site, Dr. Forbes could see that the patient had re-occluded and needed to go in to have a touch-up procedure done.
“The standard practice after revascularization is to recheck at around six months. But that would have led to a significantly worse outcome, or maybe even an amputation if we didn’t have our protocol to screen early with Snapshot,” says Dr. Forbes, who adds that information captured by SnapshotNIR is also a comfort to the vascular surgeons the team works with. “They like it because they know that the patients we send to them are not wasting their time.”
Dr. Jason Forbes and Clinical Nurse Manager, Erin Buchness.
Improving Morale
In addition to using SnapshotNIR to screen new patients, as part of the limb preservation program, Dr. Forbes and his team also use it on longer-term patients who are displaying negative wound changes or are not healing on pace.
“We have clinic goals here,” explains Buchness. “We like to see a patient healed at 50 percent within four weeks. If they have not hit that goal, then we do a repeat Snapshot to once again [gauge the level of oxygenation].”
According to Dr. Forbes, whether they’re new to the clinic or further along their treatment path, patients appreciate the information captured on SnapshotNIR and how easily translatable it is.
“Right at point of care, we can take a picture, and then we have a nice big screen that we can use to show the patient exactly where any deficits are,” he says. “So, instead of just giving patients what, in their mind, might be an ethereal concept of what’s wrong, where there might be a blockage and why it hurts, we can show them, within seconds, where their problem is, where we need to focus to achieve our healing goals, and why we’re asking them to do what we need to do, especially our hyperbaric patients.”
Dr. Forbes also sees SnapshotNIR as a tool for occasionally boosting a patient’s morale, should they start to lose hope that they’re on the mend. The device’s ability to clearly capture, record and track a wound’s size and oxygenation progression helps the patient to see and understand that they’re healing — even if it’s on a microscopic level. And for a doctor who believes deeply that positive patient relationships are integral to positive outcomes, this type of reinforcement is key.
“In wound care, it’s so important for patients to see improvement. A lot of times they just need encouragement — a high-five or a hug. But they also need to know that what they’re doing, what we’re doing together, is working. And Snapshot helps with that.”
Dr. Jason Forbes, DO
Mercy Wound Care Clinic and Hyperbaric Centre
Springfield, Missouri
GAME CHANGERS: If you would like to share your experience with SnapshotNIR through an Ask the Expert Interview or Customer Story, contact Kent Imaging via email for more details or call TF: 1-833-733-5368