Pain points in Indian Health Services (IHS) and how SnapshotNIR can help
Indian Health Services (IHS) is the principal federal health care provider and health advocate for the Native American population in the United States. It operates within the US Department of Health and Human Services and provides medical services including in-patient, ambulatory, emergency, dental, public health, and preventive health care as well as outpatient care such as screening and health education.
IHS serves approximately 2.2 million of the nation’s 3.7 million Indigenous populations, most who live on or near reservations and in rural communities in the Western United States and Alaska. They provide services through tribally contracted and operated health programs in 37 states across 26 hospitals, 59 health centers and 32 health stations.
Much like other countries, the Indigenous population in the US experience health disparities. Life expectancy in Native Americans is 73.7 years compared to the general population of the country which is 78.1 years.
In comparison on death rates, it’s also three to fives times higher for Native Americans when it comes to chronic liver disease and cirrhosis, diabetes mellitus and other preventable diseases than for other races combined. IHS serves populations that demonstrate the highest prevalence of type 2 diabetes in the world and in which cardiovascular disease is the leading cause of mortality.
The IHS faces several challenges and pain points including increased healthcare costs, need for nursing and long-term care for seniors, high financial burden, and rising rates of new diseases.
To provide effective and quality health delivery and efficient resource management, IHS has prioritised innovation in care delivery through health information technology where a key part of that is in electronic health records and telehealth. This can help address preventive and treatment needs of Native Americans.
SnapshotNIR is a mobile device that can be used in remote underserved areas where much of the Indigenous population in the United States reside. It helps healthcare workers and clinicians to capture the diagnostic insight into oxygenated blood in tissue using near-infrared spectroscopy. It also tracks and documents the effectiveness of treatment and to help assess the capacity of a wound to heal. It’s a tissue oxygenation measurement device that reports the value of oxygen saturation, oxyhemoglobin and deoxyhemoglobin levels in superficial tissue.
When used in rural and remote geographical areas that IHS serves, SnapshotNIR can provide physicians and surgeons with accurate point-of-care data. It’s a non-invasive tissue assessment device that can be used to triage patients earlier and expedite referrals to necessary specialties, including vascular.
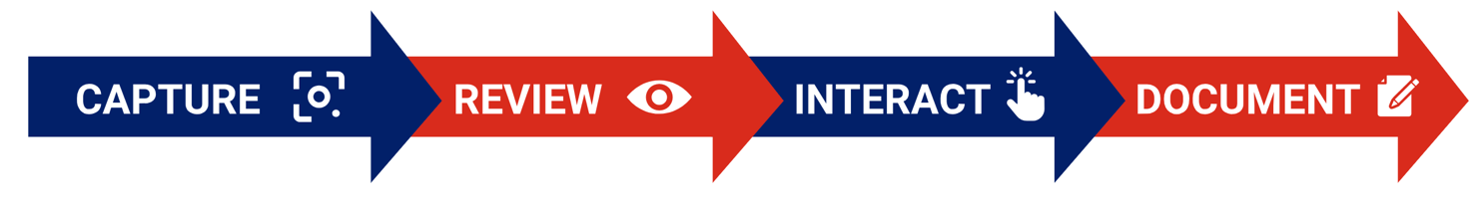
SnapshotNIR is a cost-effective, easy-to-use device that can impact treatment options and healthcare costs for systems like IHS. The device captures image reports which can be easily added into the patient’s electronic medical record and patient chart. This allows clinicians and surgeons to collaborate on care plans because information from the device allows them to rapidly assess injured tissue so they can monitor the healing process and determine if the prescribed treatments are effective or require a change in the care plan.
Previously, the equipment and procedures commonly used to obtain vascular and tissue oxygenation assessments were large, non-mobile and costly to acquire. In remote environments, outside of clinical laboratories and hospital settings, it can be challenging to obtain reliable and repeatable non-invasive vascular studies in a timely and convenient manner. The current procedures are time-consuming, require special technician training and all involve direct patient contact.
Patients accessing IHS care may have to travel to larger centers just to get properly assessed which can be costly regarding time and money. By comparison, SnapshotNIR is portable, handheld, and lightweight and images are captured without the need for patient contact. There is no per use cost and since it allows clinicians to image patients easily throughout their care, it can be applied in a variety of care settings including the ER, in clinics and for pre- intra- and post-operative assessment as well as in acute and long-term care planning.
Utilizing technology like SnapshotNIR means that the delivery of health services is made more efficient and patients can stay in their community with support from local clinicians and those at other sites. They would only need to travel to advanced centers for additional assessment when warranted, saving time and expenses. Since images from SnapshotNIR are easily and securely shared to remote locations for physicians or specialists to review, improved medical collaborations between clinicians ultimately improve patient care and outcomes.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3035828/
https://www.nytimes.com/2020/09/29/us/politics/coronavirus-indian-health-service.html#:~:text=Long%20before%20the%20coronavirus%2C%20the,hospital%20beds%20and%20aging%20facilities.
https://www.ihs.gov/newsroom/factsheets/quicklook/#:~:text=HEALTH%20CARE%20DELIVERY&text=Health%20services%20are%20provided%20directly,centers%2C%20and%2032%20health%20stations.
https://www.kentimaging.com/blo2g-articles/snapshotnir-community-based-care