Wound bed preparation for split thickness skin graft on flank wound
Presented by: Dr. Charles Andersen, MD, and Homer-Christian Reiter, BSc
Using SnapshotNIR to monitor the benefit of serial debridements using EZDebride and skin graft application
Case summary
The patient presented 2 weeks after a penetrating injury to their left flank. The wound was initially treated for infection, followed by serial debridements to prepare the wound bed for a skin graft application. Using SnapshotNIR, a near-infrared spectroscopy (NIRS) imaging device, the wound was serially debrided and imaged to ensure devitalized tissue was removed and sufficient granular tissue was present to support a graft. Serial debridements continued for one month. Other treatment interventions included wound vacuum (vac) placement and further infection control.
A split thickness skin graft was applied and demonstrated 100% take, following imaging with SnapshotNIR. At 6 months, the patient was re-imaged and demonstrated a fully epithelialized and deeply healed wound and was discharged from care.
Initial debridement on 3/15/24 on the left side of the image. Fully epithelialized and deeply healed split thickness skin graft on 10/21/24 on the right.
Patient Details
SnapshotNIR and EZDebride tool
A 34-year-old, otherwise healthy, male, presented 2 weeks after a penetrating trauma injury to the left flank by piece of wood during a parachute landing. The patient was found to have evidence of a necrotizing soft tissue infection, and a treatment plan was made to include multiple surgical debridements, wound vac placement and a graft application.
Case details
Infection control:
Patient presented continuing IV antibiotics and antifungal
Original culture positive for klebsiella aerogenes and rare enterobacter
Later cultures positive for mold with pending speciation
Once source control was obtained, the treatment plan was to prepare the wound for a split thickness skin graft (stsg) by completing serial debridements with EZDebride and monitoring the wound status and tissue viability with SnapshotNIR.
Wound bed preparation
Serial debridements with EZDebride were initiated on 3/15/24 and concluded on 3/26/24. Wound vac placement was used in conjunction between visits. Across four debridements with EZDebride, SnapshotNIR detected an average increase of 2.5% StO2 across the entire wound bed each subsequent visit.
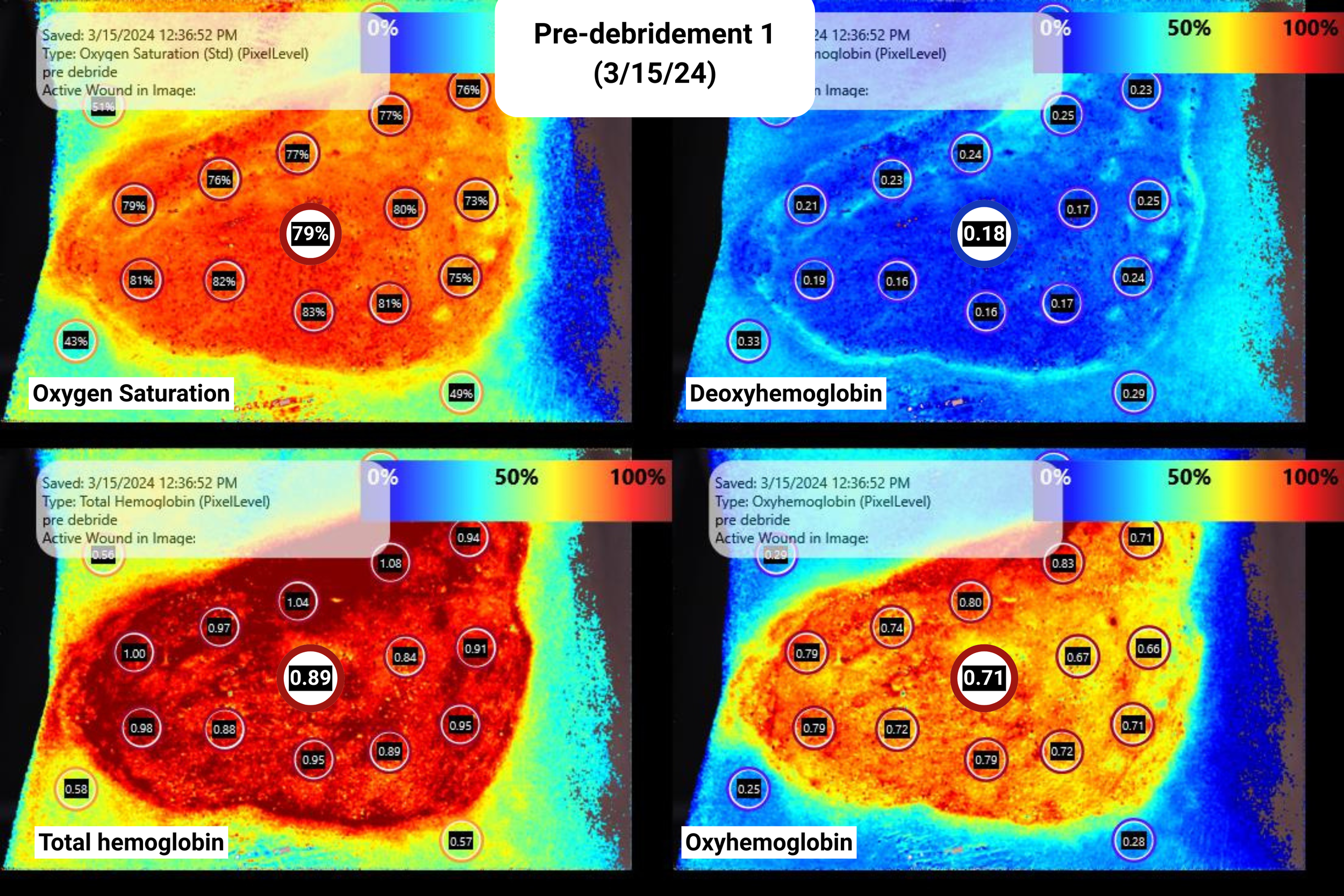
First debridement 3/15/24
Pre- and post-debridement imaging with SnapshotNIR. Post-debridement interpretations:
There was an increase in StO2
There was an increase in oxyhemoglobin
Deoxyhemoglobin had, on average, a slight decrease to no change, indicating possible minor removal of devitalized tissue
Pre-debridement, 3/15/24
Post-debridement, 3/15/24
second debridement 3/19/24
Pre- and post-debridement imaging with SnapshotNIR. Post-debridement interpretations:
A minor increase in StO2
There was an increase in oxyhemoglobin
Deoxyhemoglobin along the upper right margin of the wound was elevated, indicating the patient may have benefitted from further debridement along that margin to remove any devitalized tissue
Pre-debridement, 3/19/24
Post-debridement, 3/19/24
Fourth Debridement 3/26/24
Pre- and post-debridement imaging with SnapshotNIR. Post-debridement interpretations:
There was an increase in StO2
There was an increase in oxyhemoglobin
There was a decrease in deoxyhemoglobin
In the left center of the wound, there is small area of tissue with elevated deoxyhemoglobin indicating the patient may have benefitted from further debridement to remove remaining devitalized tissue
Pre-debridement, 3/26/24
Post-debridement, 3/26/24
Plan of care changes
EZDebride debridements and wound vac placement were temporarily paused when the patient began to grow white patches over the wound bed and there was significant concern for fungal infection. The patient was referred for bacteria cultures. No fungal growth was found by infectious disease but a heavy growth of MRSA. The patient started on linezolid 600 mg bid per infectious disease.
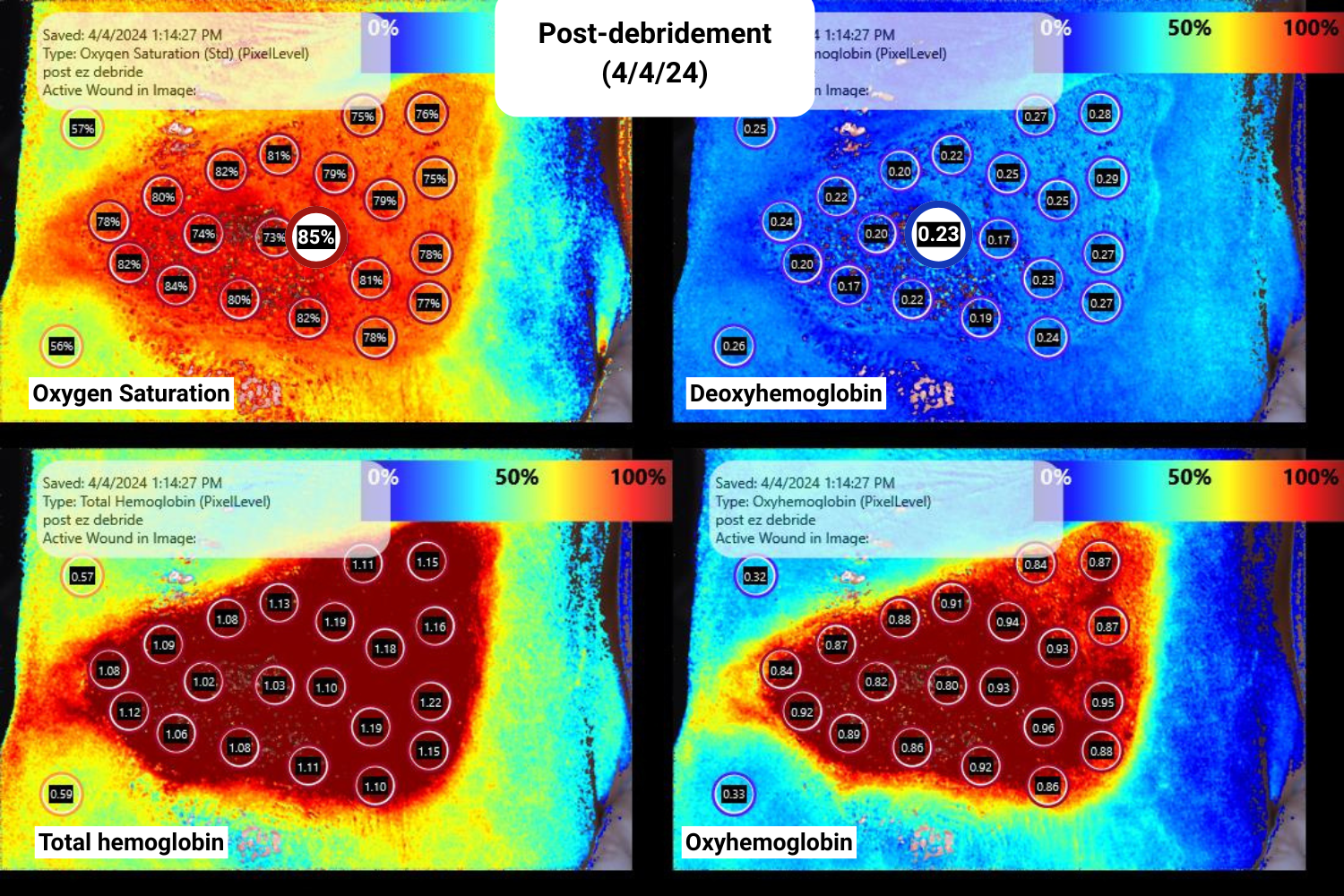
Continuation of patient care plan
After source control was reobtained, the treatment plan was resumed, and the patient resumed wound vac and debridement with EZDebride in preparation for the stsg. On 4/4/24, the patient was imaged with SnapshotNIR, which demonstrated an average 81% StO2 pre-intervention with EZDebride and an average of 82% StO2 post-intervention with EZDebride. This was the final debridement before the stsg operation scheduled for the following week.
Final debridement 4/4/12
Pre-debridement, 4/4/24
Post-debridement, 4/4/24
Split thickness skin graft application
On 4/12/24 post-stsg operation, the graft was shown to have 100% take and the wound vac was resumed. The graft adhered to the wound bed well following the serial debridements and showed good vascularization during imaging with SnapshotNIR.
Split thickness skin graft application with StO2 markers using SnapshotNIR.
Outcome of the skin graft application
The patient rapidly progressed. Visits were decreased to once per month after the wound vac removal and debridement was no longer necessary. On 10/21/24 the patient returned for follow-up. On imaging, the graft was fully epithelialized and deeply healed as confirmed by SnapshotNIR. The patient was discharged from wound care.
Deeply healed skin graft with StO2 imaging using SnapshotNIR.
“NIRS was instrumental in monitoring oxygenation of wound bed throughout serial debridements in preparation for skin grafting. Post-graft NIRS was utilized as confirmation of deep healing after epithelialization.”
Clinical images using SnapshotNIR to track and monitor patient progress and healing following a stsg application.