Wound Assessment & Monitoring with SnapshotNIR: A Focus on Debridement
What is Debridement?
Debridement is the removal of dead (necrotic) or infected skin tissue to assist with wound healing. Debridement isn’t necessarily required for all wounds but is an essential procedure for wounds that are not improving and stalled in healing. This could be a chronic ulcer that is not healing properly or a wound that has become infected. Once the necrotic tissue is removed, the wound can restart the healing process. This therapy will reduce bacteria in the wound and help healthy tissue grow.
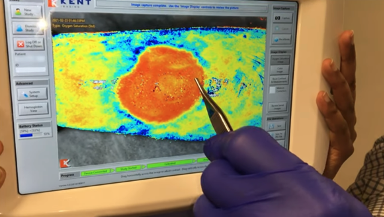
Debridement of a callus from a reoccurring ulcer. (Images courtesy of Dr. Jeffrey Niezgoda, MD)
Several types of debridement methods can be utilized in a typical wound care clinic or hospital. Usually, a combination of therapies is integrated into a treatment plan. The clinician considers what therapies are the most appropriate based on several patient factors including the wound type, the age and health of the patient, and the patient’s overall risk for complications. Debridement can be done with live maggots, special dressings, or ointments that soften the tissue. However, sharp debridement is the most common type. Sharps debridement is when necrotic or nonviable tissue is cut off or removed using a scalpel, curette, laser, or ultrasonic device.
Using NIRS during debridement interventions
Near-infrared spectroscopy (NIRS) imaging with SnapshotNIR can be used to track and document the level of oxygen saturation (StO2) and tissue perfusion in the wound bed and peri-wound. This information is used to guide a change in the treatment plan and may contribute to a more effective wound healing process.
Using SnapshotNIR during the examination allows the clinician to re-evaluate the wound post-debridement and make sure that the intervention was complete and adequate. If there are areas of poor oxygenation then additional debridement can be performed. Objective data showing the change in deoxyhemoglobin and oxyhemoglobin during serial debridements and supporting this with the oxygenation images can enhance documentation and help prove medical necessity to payors.
Pre-debridement SnapshotNIR StO2 and clinical image showing 82% StO2.
Post-debridement SnapshotNIR StO2 and clinical image showing 89% StO2.
Pre-debridement SnapshotNIR Hemoglobin View image showing 82% StO2, 0.27 deoxyhemoglobin, 1.17 oxyhemoglobin and 1.44 total hemoglobin.
Post-debridement SnapshotNIR Hemoglobin View image showing 89% StO2, 0.14 deoxyhemoglobin, 1.15 oxyhemoglobin and 1.29 total hemoglobin.
In the example above, the SnapshotNIR images show an increase in StO2 from pre- to post-debridement by 7% (from 82% to 89%) which can support the use of the intervention. For deeper insight on the effectiveness of the debridement, the clinician can check the Hemoglobin View images which will demonstrate if there was a change in deoxyhemoglobin, often indicating if there is still devitalized tissue that needs removal. In this example, the change in deoxyhemoglobin went from 0.27 to 0.14.
How does SnapshotNIR support the debridement process?
A sample debridement case study from Dr. Doug Toole, DPM., shows how SnapshotNIR can assist in charting a new course of action on a patient, saving time and money, and helping to produce a much more positive outcome for the patient.
Dr. Toole did a rapid objective assessment with SnapshotNIR on an 85-year-old female patient with a history of diabetes, vascular disease, and dementia. She presented at the clinic with a diabetic ulcer on the side of her left foot. Snapshot identified a lack of tissue viability of the foot helping to explain why the wound was not fully closing after initial treatment. With this new insight, Dr. Toole immediately altered the treatment plan to help close the wound. The new course of action included a combination of debridement and amnion injections to stimulate vascular growth.
Top (Fig 1A, 1B): Baseline clinical and StO2 images before CTP application. Bottom: One month after treatment (including debridement). Note the increase in tissue oxygenation of the wound and peri-wound sites. (Images courtesy of: Dr. Doug Toole, DPM)
Serial imaging was then performed using SnapshotNIR to track and document wound healing progress over several weeks. After a single week of treatment, the tissue oxygenation (StO2) images captured demonstrated that the area of previous concern was showing improved oxygenation. Debridement and amnion injections were continued for a month until the wound finally closed.
SnapshotNIR in clinical practice for debridement
It is portable for all points of care
An effective tool that provides actionable insight for wound debridement
Use it for rapid assessment to easily monitor the wound bed and peri-wound without the use of dyes
It can identify non-viable tissue in and around the wound bed for debridement and confirm graft survival
Use it for continual wound monitoring: clinicians can assess wound healing progress and evaluate wounds that are failing to improve
Document and track patient progress by comparing the same patient throughout their care to evaluate the effect of treatment modalities.
In the case of debridement, the economic burden of a failed CAMPs (cellular, acellular, and matrix products) application is high, both from the cost of the product and the extended period it will take to heal the wound. SnapshotNIR is the best assessment device to determine if the wound bed is fully prepared after debridement and viable for the successful application of a CAMP.
Visualizing the tissue oxygenation levels of a wound bed after debridement using SnapshotNIR prior to applying a CAMP to a traumatic leg wound. (Image courtesy of Dr. Jeffrey Niezgoda, MD)
References:
Wound Debridement, https://www.healogics.com/wound-care-patient-information/wound-debridement/
Web CME, WCW: Applying a Kerecis Graft to a Traumatic Wound (SnapshotNIR), Dr. Jeffrey Niezgoda
Web CME, WCW: Serial Debridement of Heel Eschar, Dr. Jeffrey Niezgoda
To read more about the science behind SnapshotNIR and to watch an explainer video, click here.
Original article written on August 3 2022. Updated on April 2 2025.