USING SNAPSHOTNIR TO ASSESS HBOT FOR WOUND HEALING
Presented by: Jonathan A. Niezgoda, CHWS, and Jeffrey Niezgoda, MD
PATIENT HISTORY
54-year-old female, non-smoker, non-diabetic, taking no chronic medications, presented for evaluation and consideration of hyperbaric oxygen therapy (HBOT). This was following the development of tissue ischemia and necrosis of the distal tip of D3 along with incisional ischemic compromise after a podiatric surgical intervention for the correction of foot deformities and bunions.
CASE DETAILS
Podiatric surgery was performed under regional anesthesia using a tourniquet for hemostasis which was applied proximal to the calf. The surgical procedure exceeded 2 hours due to minor intraoperative complications. The patient was discharged home after recovery and developed severe left foot pain during the night prompting a next day’s visit with her podiatric surgeon for evaluation. Dusky changes were noted over the left foot after a comprehensive exam and the patient was sent home for a repeat follow-up in 2 days.
Following up, on postoperative day 3 (POD#3), the patient was identified with necrosis of the distal tip of D3 along with incisional ischemic compromise. Based on evolving tissue necrosis, the patient was referred for vascular consultation. The vascular evaluation found absent dorsalis pedis pulses by using Doppler. The patient was then scheduled for an urgent arteriogram. Angiographic findings revealed occlusion of the dorsalis pedis artery which was thought to be related to embolization phenomena caused by the tourniquet application. The successful intervention of the dorsalis pedis artery was accomplished with recanalization and restoration of blood flow through the planar arch.
OBSERVATIONS
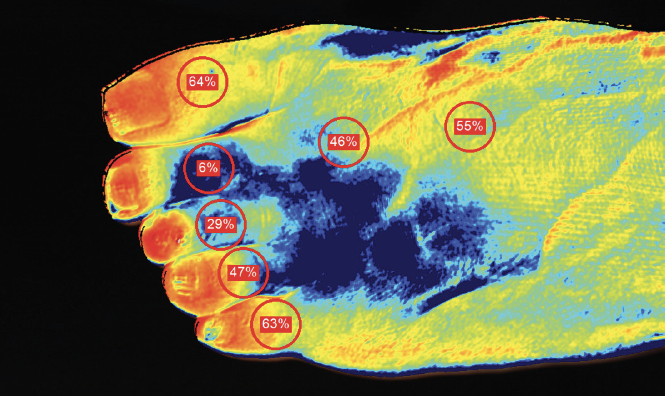
NIRS imaging with SnapshotNIR demonstrated the improvement in StO2 following the vascular intervention. However, there was still some concern based on overall depressed StO2 values in the setting of tissue necrosis. The patient was offered HBOT based on the diagnosis of acute arterial insufficiency and NIRS images were obtained pre-and post-procedure.
Significant improvement in oxygenation was observed following HBOT and the patient reported improvement in her pain following HBOT and vascular intervention. HBOT was continued and the patient was monitored serially. The patient continued to show improvement over the next several weeks and the suspected necrosis of D3 ultimately proved to be only superficial tissue loss, which was predicted through the NIRS images. Several weeks past the initial event, the eschar managed to slough, and the entire digit survived and remained viable. The patient was very pleased with this outcome.
Fig 4B. 7/21/2019: StO2 image of the dorsal surface of foot post-22 sessions of HBOT and vascular intervention.
IMPACT
SnapshotNIR was used during the initial evaluation of this patient to assess tissue perfusion and the magnitude of the ischemic compromise over the entire lower extremity. These findings were corroborated with duplex ultrasound and further supported by angiographic findings. Following the intervention, Snapshot was used to assess the patient’s response, which showed quantifiable improvement. In conjunction with HBOT, Snapshot was used to determine the response to the therapy as well as to support the continuation of HBOT. Pre- and post-images taken by the device were used to track the patient’s response over the course of HBOT. Once the patient demonstrated stabilization of her improved tissue oxygenation and clinical appearance, HBOT was suspended. A total of 22 HBOT sessions were administered, and complete healing followed 2 months later.
“The use of NIRS, in this case, demonstrated the improvement in StO2 values following vascular intervention and HBOT. Significant improvement in StO2 pre- and post-HBOT treatment 1, as well as serial improvement over time, correlating positively with the clinical impression that digit salvage effort was possible. This strategy prevented a digit amputation for the patient.”