USE OF SNAPSHOTNIR IMAGING TO EVALUATE MICROCIRCULATION OF DAMAGED LYMPHATIC PATHWAYS IN POST-MASTECTOMY BREAST CANCER
Presented by: Danae Kissner: PA-C, CWS, CLT
PATIENT DETAILS
An 81-year-old female patient was admitted to a skilled nursing facility with secondary lymphedema due to breast cancer with a left-side mastectomy/surgical debulking 30 years previously. The patient had received chemotherapy and radiation and is currently in remission. She was previously treated with complete cecongestive therapy (CDT) and compression. During her initial consult, the patient disclosed that her left upper extremity (LUE) lymphedema had not been treated for several years due to a lack of resources and non-adherence to therapy. The patient was also experiencing extensive vasculopathic and immune-compromising health issues, including DMT2 with poor glycemic control, peripheral vascular disease (PVD), coronary vascular insufficiency, morbid obesity, stable congestive heart failure, and COPD managed by her PCP (stable without O2 support and latest brain natriuretic peptide at normal levels).
CASE DETAILS
After ruling out contraindications to lymphedema management, a trial of conservative decongestive lymphedema therapy (DLT) was implemented, including elevation, muscle pump/deep abdominal breathing, and compression wraps. Despite DLT, the LUE edema remained poorly controlled, so IPC was started using an LUE sleeve with monthly clinical assessments. These assessments included near-infrared spectroscopy (NIRS) imaging with SnapshotNIR and limb measurements. NIRS imaging results showed improved microcirculation that progressed from 65% after 1 month of IPC to 79% after 2 months of treatment.
The care team reported increased congestion in LUE due to axillary and watershed insufficiencies after 3 months of IPC therapy and upgraded her to a vest sleeve for IPC. Preliminary vest IPC data from NIRS imaging showed improvement from an average of 67% to 79% microcirculation LUE, post 25min IPC compression at 48mmHg using the compression vest.
After approximately 20 minutes of IPC using the vest sleeve at 48mmHg, NIRS imaging data showed a significant decrease in the saturation of deoxyhemoglobin and a leveling out of the oxyhemoglobin levels, indicating improvement of capillary vascular and lymphatic microcirculation due to decongestion therapy and decreased tissue edema.
IMPACT
NIRS imaging and interpretation can be a useful tool to help identify microcirculation insufficiencies due to secondary lymphedema as well as to monitor the efficacy of lymphedema management, specifically DLT and IPC treatment. Using NIRS imaging to assess lymphatic watershed assessments before, during, and after IPC treatments can also help identify the need for more aggressive IPC compression that would require larger surface area IPC sleeves for upper extremity lymphedema/post-mastectomy breast cancer patients.
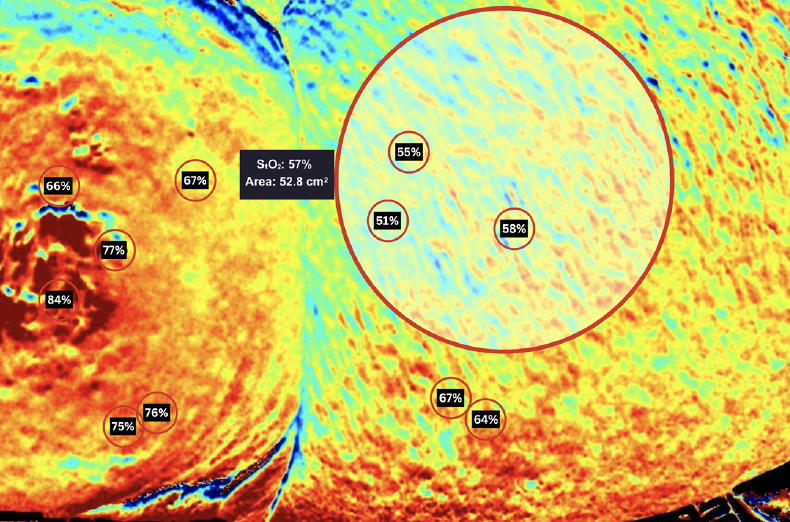
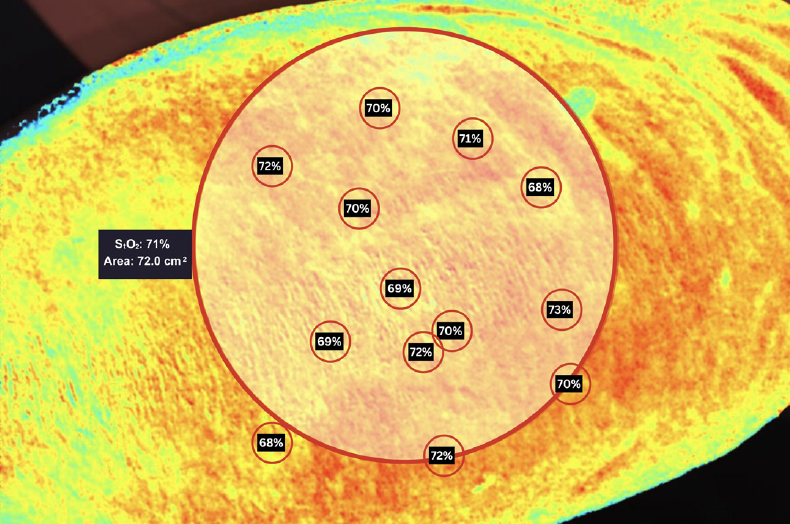
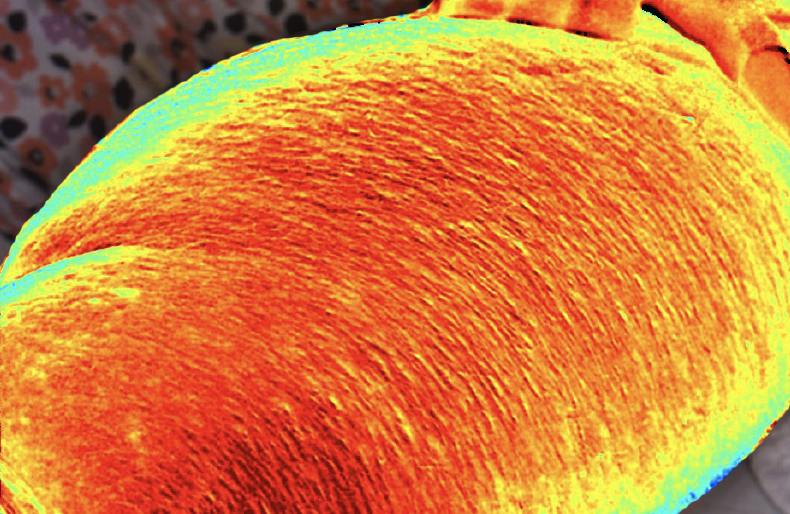
Fig 1A: Left upper arm pre-vest IPC therapy.
Fig 1B: Left upper arm post-vest IPC therapy.
Fig 1C: Left upper arm one week post-vest IPC therapy.
“SnapshotNIR helped to identify the need for more aggressive lymphedema management to assist in lymphedema watershed transport when conservative treatments were no longer effective. Periodic Snapshot assessments, in conjunction with routine delimb circumference measurements, helped monitor the efficacy of IPC.”
