VASCULAR SCREENING / PRE & POST VASCULAR INTERVENTION
Dr. Charles Andersen, MD, FACS, MAPWCA
Chief of Vascular/ Endovascular/ Limb Preservation Service at Madigan Army Medical Center in Tacoma, WA Homer-Christian Reiter BSc
Research Coordinator at the Geneva Foundation in Tacoma, WA
PATIENT HISTORY
A 66-year-old female patient with type II diabetes, hypertension, morbid obesity and no known history of peripheral arterial insufficiency was being seen by neurology for leg pain. She was referred to the wound care clinic for a wound secondary to a biopsy that was failing to heal and enlarging in size.
CASE DETAILS
The patient presented to the wound clinic with a 7.25 cm3 wound on the left lateral leg and pain in her legs that was thought to be neurologic. The wound had erythema at wound edges and was ischemic looking with slough in the base of the wound. At the initial wound care clinic visit, the combination of physical exam, doppler evaluation and NIRS, were used at point-of-care to evaluate the limb for arterial disease. Doppler results were monophasic to biphasic. A leg elevation challenge was used in conjunction with the NIRS for the evaluation of arterial status. When comparing the supine NIRS image to the elevated leg NIRS, a significant drop in oxygenation was apparent. Based on the initial evaluation, severe arterial disease was suspected and the patient was referred for further vascular studies. Vascular disease was also felt to be the cause of the leg pain. On day 6, non-invasive vascular studies were performed with the following results:
• ABI on right PT=.35, DP =.31
• Left PT was not obtained, DP=.24
• The patient had bilateral flat toe waveforms
The right and left ABIs and toe waveforms were consistent with severe arterial insufficiency and the patient was scheduled for an arteriogram and subsequent bilateral common iliac artery stenting.
RESULTS
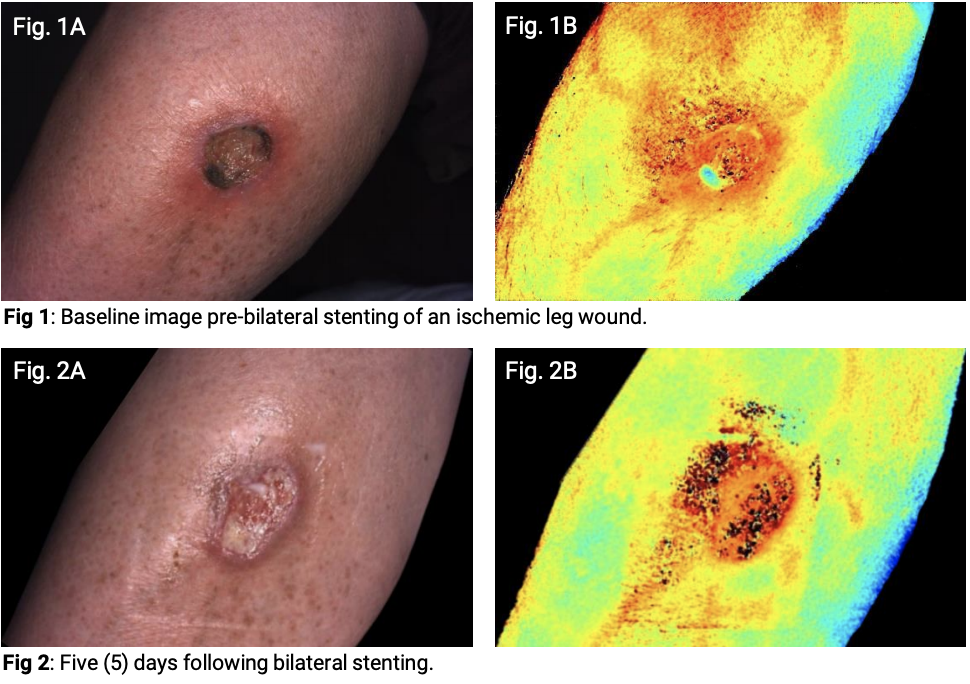
On Day 28, bilateral stenting was performed to correct high-grade stenosis in bilateral common iliac arteries. Post-procedure palpable pulses were found in CFA, PT, and DP bilaterally. NIRS imaging was performed approximately 60 minutes post-procedure. The images obtained showed immediate improvement. At the follow-up visit 5 days later, a doppler was performed and a tri-phasic signal in both feet was found. NIRS images were captured that continued to show and document vastly improved oxygenation, even with the elevation challenge. The wound volume at the latest visit had reduced in size to 3.08 cm3.
IMPACT
Utilizing the Snapshot NIRS images on the initial evaluation in the wound care study, severe arterial disease was documented, leading to subsequent vascular evaluations and treatment.
“Snapshot images can be a very important part of the screening in the wound care clinic.”